The need for frequent injections, along with the associated cost and travel time, is a big challenge for people with neovascular age-related macular degeneration, their caregivers and their ophthalmologists.
A new drug that extends the interval between injections has been found to meet safety standards and efficacy targets, and should be available in Australia in late 2018 or mid-2019.
The first human trial results for the drug showed a median extension of 30 days between injections. This virtually doubles the safe treatment intervals required for currently available treatments. The drug also reduces the thickness of the central macula fluid.
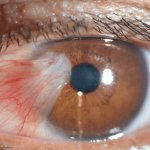
With age-related macular degeneration, a chemical known as vascular endothelial growth factor, or VEGF, causes abnormal blood vessels to grow under the retina. Current treatments, known as anti-VEGF drugs, block this chemical, slowing the loss of vision.
The new drug is the smallest of the anti-VEGF antibodies. A single injection can deliver 6 mg—this is 12 times more than aflibercept (Eylea®) and 22 times more than ranibizumab (Lucentis®).
The treatment cycle needs to be customised for each patient. We will learn more once the drug is released.
If you are experiencing blurry vision, make sure you see your optometrist to have your eyesight checked.
https://www.ncbi.nlm.nih.gov/pubmed/28551167
http://www.sciencedirect.com/science/article/pii/S0161642016324137